A 34-year-old mother and police officer died after doctors declined to provide urgent cardiac treatment once they learned she was pregnant.
The case is now fueling concern in the U.S. over how abortion restrictions are reshaping medical care for high-risk patients.
Ciji Graham, a Greensboro, North Carolina-based police officer and mother of a two-year-old boy, sought medical help on November 14, 2023, after her heart rate surged to a life-threatening 192 beats per minute.
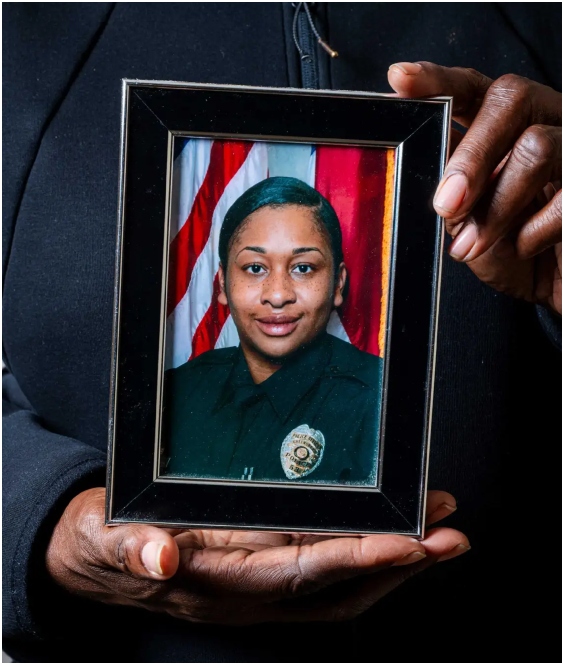
Diagnosed with atrial fibrillation, Graham faced a high risk of stroke or heart failure. In previous episodes, doctors had successfully restored her heart rhythm using cardioversion, a procedure widely considered safe even during pregnancy.
This time, however, her care stalled.
According to a ProPublica investigation authored by Lizzie Presser and Kavitha Surana, Graham was denied cardioversion after a pregnancy test came back positive. Medical records show she was sent home and instructed to consult multiple specialists, despite ongoing symptoms including chest pain, breathlessness and severe palpitations.
Global medical consensus, including guidance from the Heart Rhythm Society, holds that cardioversion is both safe and effective during pregnancy. More than a dozen cardiologists and maternal-fetal medicine specialists interviewed by ProPublica said Graham should have been immediately admitted to hospital for treatment.
Instead, she was caught in a dangerous gap between medical caution and restrictive abortion laws.
North Carolina bans abortion after 12 weeks and has imposed additional procedural hurdles, including mandatory waiting periods. Though Graham was only about six weeks pregnant, she struggled to find a provider willing and able to intervene quickly. Clinics were overwhelmed, hospitals were reluctant to discuss abortion-related care, and no physician stepped in to coordinate her treatment.

As her condition worsened, Graham came to believe that ending the pregnancy was the only way to save her life. Yet even that option proved elusive. She was forced to wait nearly two weeks for an appointment, despite her deteriorating health.
On Nov. 19, 2023, Graham was found dead in her apartment. The medical examiner ruled her cause of death as cardiac arrhythmia due to atrial fibrillation in the setting of recent pregnancy. No autopsy was conducted.
Experts who reviewed her case concluded that her death was preventable.
“She should never have been sent home,” said one cardiologist consulted by ProPublica, echoing broader concerns that fear of legal repercussions is leading doctors in some U.S. states to delay or deny standard care to pregnant patients.
Graham’s death is one of several investigated by ProPublica involving women who died after being unable to access timely medical treatment in states with strict abortion laws. The United States already has the highest maternal mortality rate among wealthy nations, more than double that of countries such as the United Kingdom, where high-risk pregnancies are centrally managed under national protocols.
For audiences in Ghana and across the Global South, Graham’s story underscores how legal frameworks, even in advanced healthcare systems, can profoundly affect patient outcomes. It also highlights a growing international debate about whether laws intended to protect life are, in practice, placing vulnerable women at greater risk.
Graham left behind a young son, SJ, who has been told that his mother has gone to the moon. Each night, he points to the sky and tells her he loves her.
Her family and medical experts say she should still be alive.